INTERVERTEBRAL HERNIATION (Hernia of intervertebral disk)
Alternative names: intervertebral hernia, disc herniation of the spine, a herniated disc, prolapse of the disc.
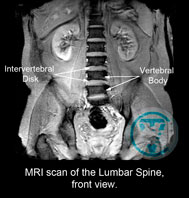
The spine consists of the vertebrae and disks. The intervertebral discs are located between the vertebral bodies. Their main function is the cushioning of the spine during physical activity and ensure the stability of the adjacent vertebrae in the spinal motion segment (SMS), in other words: functional spinal unit (FSU). In addition, owing to their elasticity, the discs are the major factor of determining the flexibility of the spinal column.
(SMS or FSU is a term denoting a functional unit of the spine and represents the articulation of two adjacent vertebrae with the disc between them plus the surrounding ligaments and muscles).
Human body has 23 intervertebral discs. The first is between the bodies of the second and third cervical vertebrae (C2-C3) and the last is between the bodies of the fifth lumbar vertebra and first sacral (L5-S1).
Anatomically, they are represented by fibrous and cartilaginous substance as a discoid shape (hence the name is). The disc's diameter is about 40 mm. The thickness of it depends on the part of the spinal column, (on average is 4-10 mm). The largest disc size is detected in the lumbar spine, the smallest is in thoracic spine.
The disc consists of three parts: a very strong fibrous ring (annulus fibrosus), inside of which is lying gelatinous (jelly-like) substance, which is called the nucleus pulposus. It is believed that the core is the main absorber of the spine. Inter-vertebral discs separated from the vertebral bodies by a thin hyaline cartilage (end plates of vertebra). They have a dual purpose: on the one hand, they protect the spongy bone of the vertebral bodies from excessive pressure caused by the nucleus pulposus during the load and on the another hand, the cartilage plates of the inter-vertebral discs receive nutrients and they continuously renew the liquid portion of nucleus pulposus.
It is considered that the core of intervertebral disc is the main shock absorber of the spine.
From the adjacent vertebral bodies, intervertebral discs are separated by a thin hyaline cartilage (end plates). These end plates have a dual purpose. On one hand, they protect the cancellous bone of the vertebral bodies from excess pressure coming from the nucleus pulposus when a heavy load is applied. And, on the other hand, through the cartilage plates in the intervertebral disc, nutrients are received, and there is a continuous update of the liquid portion of the nucleus pulposus. The chemical exchange in the disc visibly improves during movement of SMS by increasing blood flow to the surrounding muscles and ligaments as it doesn’t possess its own vascular system.
The innervation of the intervertebral disc happens due to the autonomic nervous system. Metabolic disorders have a negative effect on the connective tissue structure of the disc, reducing the strength of the fibrous ring. Herniated disc (HD) is a condition when there is a rupture of the fibrous ring of the nucleus pulposus and beyond its boundaries. With the loss of the liquid contents, the vertical size of the disc is reduced. This leads to the convergence of the vertebrae to strengthen the facet joints when there is a load put on the spine. Migration of the disc’s contents, as a rule, is usually accompanied by aseptic inflammation, muscle tension, swelling, and pain.
In cases where there is penetration of fragments of the nucleus pulposus through the damaged endplate in the vertebral body suggest hernia Shmorlya. With such a painful process, the disc is not displaced in relation to the above and below laying vertebral bodies, and has no effect on the nerves or the spinal cord.
The illness (HD) is preceded by a disc protrusion—a disc with one of its sides bulging. During this, the displacement of the nucleus pulpous doesn’t occur beyond the fibrous ring.
It is believed that the cause of the spinal disc herniation is osteochondrosis, spinal curvature (scoliosis, kyphosis, lordosis), weakness of the surrounding muscles, excessive heavy lifting, sedentary lifestyle, being overweight, and/or combination thereof. However, there is evidence (Bengus L.M., Dedukh N.V., 2012) that preceded the appearance of hernia degenerative changes of the fibrous ring due to the disturbance of the feeding of disc while a heavy load on the spine is the cause. In this case, the degree of the load may not exceed the typical amount for that person. Thus, the main causes of spinal disc herniation are: osteochondrosis, the trophic systems disorders of the disc, and chronic, local overload of the spine. Via localisation, you can distinguish different types of hernia in the cervical, thoracic, and lumbosacral parts of the spine. In some cases, the disc prolapse can be in several areas (e.g. in the cervical and lumbar), which isn’t so rare.
Hernia of the cervical spine, according to various sources, can appear 4-19%. It is believed that the cause of a cervical osteochondrosis is the prolonged stay in a static position with an offset head forward. This leads to increased cervical lordosis, long-term overload of the neck muscles, compensation of the nerve roots and intervertebral disc deformation (e.g. when working on the computer). Clinically speaking, the disease can manifest as a pain in the neck, stiffness of muscles, headaches, dizziness, unstable blood pressure, problems with the sensitivity in the upper limbs, etc. The symptoms characteristic of cervical osteochondrosis and “symptoms of loss” are observed during the compression of the nerve root.
The thoracic spine hernia appears 2-30% of the time. There are constant chest pains that increase during movement.
60-85% of lumbosacral hernia cases are associated with the highest load on the spinal column. It can manifest and form into lumbodynia—a dull, aching pain in the lumbar region that increases during exercise. The pain may spread to the buttocks area, back of thigh, and lower leg. This is characteristic to the sharp increase in pain when coughing and sneezing. To reduce the pain, patients were forced to adapt an antalgic posture (reflective scoliosis). In addition to these symptoms, there may be numbness in the lower extremities: numbness, tingling, burning. Trophic disorders manifest as loss of muscle mass and decreased muscle strength. The disturbance of innervation may be one of the causes of the disease of large joints (knee and hip) with development of deforming arthrosis (gonarthrosis and coxarthrosis). In severe cases, this impairs the function of the pelvic organs (Cauda equina syndrome, CES) with urination disorder, bowel movements, and can cause paralysis of the lower limbs. There is also a decrease of potency in men. To reduce pain, patients were forced to take a gentle pose or antalgic posture (reflexive scoliosis). Various clinical manifestations of intervertebral hernia of the lumbar spine.
To reduce pain, patients were forced to take antalgic posture, gentle posture – (reflexive scoliosis.)
Various clinical manifestations of intervertebral hernia of the lumbar spine.
DIAGNOSTICS
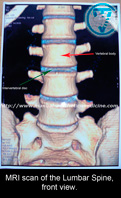
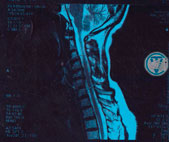
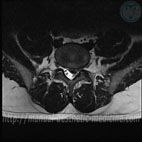
The most important method of diagnosis of an intervertebral hernia is a Magnetic-Resonance Imaging (MRI). This method allows for accurate diagnosis of the presence of an intervertebral hernia, its location, size, as well as the condition of the spinal canal, and the presence of complications. In order to determine the conductivity of nerves, suffering from hernia compression, electromyography is used.
Treatment
There are two directions in the treatment of spinal disc hernias: conservative and surgical. Many authors agree that the disease can be successfully treated with conservative methods.
The main objective of the surgery, when there is a prolapse of the intervertebral disc, is removal of the spinal cord compression or end “horse tail”. This releases the nerve roots and blood vessels in the foraminal openings and relieves pain. However, the operation does not eliminate the root cause of the disease—osteochondrosis remains.
We believe that the disease (HD) should be considered as a system (23/02/2016), at the heart of which lies degenerative-dystrophic changes in the connective tissue in the fibrous ring of intervertebral discs. This is confirmed by the presence of multiple hernias in the same patient, which doesn’t happen often. Therefore, a local surgical treatment isn’t always effective.
According to statistics, 98% of patients feel better for a short time after the surgery. After a while, their condition worsens and the disease progresses. Furthermore, during the operation, it is necessary to dissect ligaments that support the spine. As a result, the risk of new hernias appearing increases. Based on the data, Habirov F. A. (2000), various complications occur after the removal of disc herniations four out of five times. Murtagh J. (2007) believes that surgery should be performed no more than on 2% of patients suffering from lower back pain. Ya. Yu. Popelyansky (2011) suggests even lower figures of 0.3%.
To summarise, the arguments against the surgery are:
* The operation doesn’t eliminate the root cause of the disease.
* There is a high probability of relapse and re-emergence of a new hernia.
* Possible post-operation complications (adhesions, scarring, secondary spinal stenosis, fistulas).
* Blocking or instability in the operated as well as in the lying
above and below SMS-(spinal motion segment).
* Elimination of pain can’t be guaranteed.
At the same time, we are not talking about cases where there are signs of compression of herniated spinal structures and elements of the cauda equina with the threat of paralysis and dysfunction of the pelvic organs (Popelyanksy Ya. Yu. 2011).
Although hernias rarely require surgery, in the USA over 200,000 people, and 20,000 in Germany, annually undergo this operation.
The method we use allows for the manipulation of both, the entire spine and within one individual SMS. With careful manual traction, it is possible to obtain negative pressure in the damaged disc area that provides absorption of the herniation (manual traction eliminates the danger that, not infrequently, is accompanied by the mechanical stretching of the spine). Reducing the size of the hernia gets rid of the compression of nerve structures in the affected segment, the debilitating pain becomes bearable or disappears, tense muscles relax, and microcirculation is restored in the adjacent tissues. All these conditions are created for the regeneration of the disc.
With separate methods of manual therapy, it is possible to remove the subluxation of the articulationes zygapophysiales joints, remove the pressure from the affected segment, which also helps to reduce pain and reflex correction of scoliosis. To consolidate the therapeutic effect of manipulation, it is advisable to carry out on a daily basis.
The unabsorbed part of the hernia dissolves (broken down by macrophages) and the area of the disc rupture is closed with scar tissue (sanogenesis occurs).
Articulationes zygapophysiales joints, remove the pressure from the affected segment, which also helps to reduce pain and reflex correction of scoliosis. To consolidate the therapeutic effect of manipulation, it is advisable to carry out on a daily basis.
The unabsorbed part of the hernia dissolves (broken down by macrophages) and the area of the disc rupture is closed with scar tissue (sanogenesis occurs).
The acute pain is not a contraindication of manipulation. Along with manual therapy, the medications we prescribe help reduce the pain and inflammation. Injectables are usually introduced by mesotherapy or via Magnetophoresis.
Unsafe treatment techniques
The following methods are unsafe treatments in manual therapy in cases of disc hernia. The unsafe methods that are commonly employed by practitioners are methods such as the twisting of the spine, various hits with the fist, and pushing or applying rough pressure onto the spine. Such techniques can increase the expulsion of the disc’s inner gel-like center, the nucleus pulposus, provoke pain, muscle spasm, and significantly worsen the patient’s condition. Roughly speaking, such rough manual techniques on the spine, particularly in cases of disc hernia, can be considered as "SPINAL TERRORISM" and should not be applied.
Rough manipulative techniques on the spine in cases of disc hernia, can be considered as "SPINAL TERRORISM"
Misconception
In common parlance, it is often referred to as an intervertebral hernia falling out, hence the widespread misconception that the disc can be “put back” in the “right” place. To insert or right the hernia’s protrusion is impossible. For the simple reason that the disc is not available for manual exposure (just look inside an anatomy textbook), and a distinctive sound, although often present during manipulation of the spine which comes from the facet (intervertebral) joint, has no relation to “repositioning” of the disc. In addition, as noted above, the hernial protrusion is a jelly-like formation which, at any pressure to it, simply spreads to exacerbate the problem.
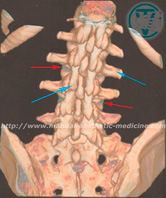
MRI image of the lumbar spine from the back. Red arrows mark small fragments of the intervertebral discs.
Blue arrows mark the processes of the vertebrae.
Numerous processes of the vertebrae, and the powerful muscles
of the back that cover the intervertebral discs, therefore, direct manual exposure is not available.
Feedback from our patients:
Additional pages:
Intervertebral herniation (Hernia of intervertebral disk) Arthrosis deformans of the hip and knee joints (Gonarthrosis) CoxarthrosisSciatica Re-Alignment and Reduction (Vertebral-fat pad, Buffalo Hump) Neck Osteochondrosis (Cervical spondylosis) Carpal tunnel syndrome (Is there a need for an operation?) Visceral Manual Therapy (Key method) SELF-MASSAGE ORGANS OF THE CHEST CAVITY DEFORMATIONS OF FOOT AND TOES
The following are problems my treatment can help with:
- Headaches
- Pain in all parts of the back
- Weak Limbs
- Joints Pain and Stiffness
- Prevention and treatment of problems caused by disc hernia
- Sport Injuries
- “Frozen Shoulder”
- Cellulite and Localised Fat reduction
- Correction of Figure
- Treatment of acne on the face and back (the original technique)
- Asthma
- Chronic Constipation (Treatment)
Manipulation is also possible on the elderly and on pregnant women.
Dr. Vladimir Tolkachov. A man with anaesthetic in his hands...Marty Mc Cool